From l to r: Dr Jill Madine, Dr Riaz Akhtar, Professor Francesco Torella (Vascular surgeon, RLUBHT) and Ian Brunell.
It may be the most romantic day of the year, but for Dr Riaz Akhtar from the University’s School of Engineering and Dr Jill Madine, from the Institute of Integrative Biology, today is just another day in the lab, studying a life-threatening heart condition.
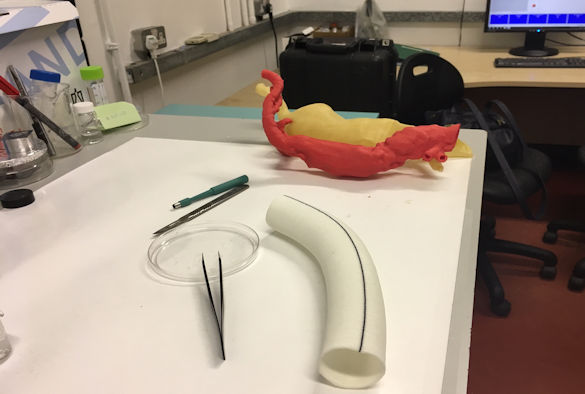
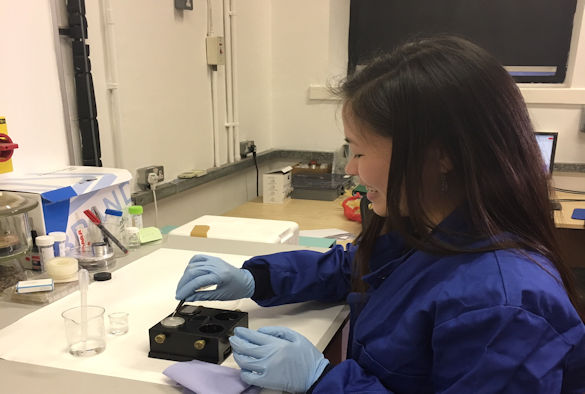
Dr Akhtar (below) and Dr Madine work jointly on a project, funded by the British Heart Foundation, which is developing a new method to assess patients when the main artery in their chest becomes dangerously enlarged, a condition known as a thoracic aortic aneurysm.
The aorta is the biggest blood vessel in the body, and is the artery which takes oxygenated blood from the heart to the rest of the body.
An aneurysm, or swelling in the blood vessel, can happen anywhere along the aorta, but a thoracic aortic aneurysm – that occurs in the section of the vessel within the chest – is of particular concern, as it is very difficult to detect, and occurs in younger patients without prior symptoms. If it is untreated or unrecognised it can rupture and cause near instant death.

Explaining why his research is important, Dr Akhtar said: “At the moment, size is one of the main measures used to determine when an aneurysm is likely to burst. However, in some patients the aorta may burst at a smaller size or the patient may develop an aortic dissection. A dissection is where a tear develops in the wall of the aorta. The wall then separates in to two layers leading to blood flowing inside the wall. An aortic dissection is an emergency, life-threatening condition.
“Currently, size is the only measure which is used to determine when an aneurysm is likely to burst: an emergency, life-threatening situation called an aortic dissection. What we know, from our research, however, is that sometimes the aorta ruptures before it gets to this size, so size alone is not an accurate enough gauge of risk.
“We are using a range of data to look at other ways to spot high-risk patients, in order to get them the surgery they need before their situation becomes critical.”
Aortic dissections became national news when former Liverpool FC Manager Gérard Houllier was rushed to hospital after this condition caused him to collapse during a game in 2001, and required 11 hours of life-saving surgery.
“We never want patients to have to experience this trauma,” Dr Akhtar continues, “the surgery to correct a dissection is extremely complex, and sadly many people will not survive. Our research is aiming to prevent this heartbreak, and ensure aneurysms are caught before the situation progresses to this stage.”
Dr Akhtar saw the anguish that aortic dissections can cause, when his friend and former colleague at the University of Liverpool, Ian Brunell, nearly lost his life to the condition.
Now 47, Ian has had a series of operations on his aorta over the last 17 years, including emergency surgery to fix an aortic dissection when he was working in Germany, in 2005:
“I was working on a Sunday, catching up on some bits and pieces, when I felt a very strange sensation – like a zip being opened in my chest. It turned out I was having a dissection of the descending aorta.
“This is a very serious condition and a lot of people don’t even make it to hospital alive when it happens. I was very lucky to survive, but the experience was very traumatic, and afterwards when I returned home to Liverpool, I ended up suffering with mild depression and post-traumatic stress disorder (PTSD), which required 6 months of therapy.
“Following that, I had surgery to replace my descending aorta. The surgeon doing the operation said that it would be the ‘surgical equivalent to being hit by a bus’ – it’s basically a very serious operation.
“The work that Dr Akhtar and Dr Madine are doing could prevent people like me from experiencing this sort of trauma. It’s not only been very difficult for me, but for my parents and friends who have had to stand by and watch as I have nearly died a number of times. Providing a new way to assess risks and intervene before a patient becomes so seriously ill will reduce the heartbreak felt by loved ones.”
Dr Akhtar was provided a £155,355 grant by the BHF in 2017 to work on this project. Local BHF Fundraising Manager Hayley Gough says fundraising is vital to supporting research:
“1 in 4 people in the UK die from heart or circulatory disease. For over half a century the BHF has been working with scientists across the country to improve outcomes for patients suffering with these conditions – but there is still more work to be done.
“We are currently funding more than £22 million of research in over 70 projects in the north-west of England. Only with the help of our supporters can we continue to fund life saving research and beat heartbreak from heart and circulatory diseases, forever.”
To find out more about research funded by the BHF, visit www.bhf.org/research