Researchers from the University of Liverpool are helping with a collaborative research study that aims to identify early warning signs of health deterioration in children.
The Dynamic Electronic Tracking and Escalation to reduce Critical Care Transfers (DETECT) study has been funded by a £1.25m grant awarded by the National Institute for Health Research Invention for Innovation Programme (NIHR i4i).
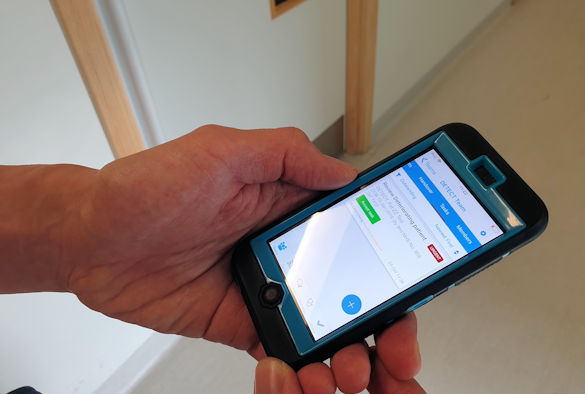
Staff at Alder Hey Children’s Hospital are currently using the electronic hand held devices to record patient vital signs (breathing rate, effort of breathing, oxygen saturation, oxygen requirement, heart rate, blood pressure, capillary refill time, temperature) and nurse or parental concerns
The recorded data will automatically calculate a paediatric early warning score (PEWS), which categorises the risk of developing serious illness into low, medium, high or critical.
UK first
This is the first large study of its kind in children in the UK to evaluate the effectiveness of an electronic physiological surveillance system, incorporating both an age-specific Paediatric Early Warning Score (PEWS) and the National Institute for Health and Clinical Excellence (NICE) sepsis screening guidance.
It is a collaborative study involving researchers from The University of Liverpool, Edge Hill University, The University of Lancaster and the healthcare IT company System C.
PEWS lead at Alder Hey Gerri Sefton said: “Developing an early warning system for children is much more complex than for adults.
“Children’s rate of breathing, heart rate and blood pressure alter significantly from birth to adulthood, so the model we use to judge how unwell a child is has to change with age. Children require five different age specific risk models, while adults have just one.”
Ongoing challenge
This technology automatically loads the correct age-specific PEWS risk model associated with the patient’s date of birth, by reading the barcode on their hospital ID band.
The technology uses CareFlow Vitals software platform (formerly known as VitalPAC), which was shown to improve serious illness recognition and reduce deaths in adults. Vitals works in tandem with Careflow Connect which is a secure encrypted communication system for health professions. Connect provides automated alerts about the sickest children and includes the ability to escalate concerns direct to the clinical team, without the nurse leaving the patient’s bedside. Push notification of laboratory results help to identify when a child might have sepsis, a serious illness associated with an overwhelming response to infection.
The early identification of clinical deterioration in children is an ongoing challenge across the NHS. Children cannot easily communicate that they are very unwell, and rely on adults to notice the subtle signs. Children in hospital who become critically unwell and require emergency admission to critical care, are sicker, need more intensive treatment and have a longer hospital stay compared to other admissions.
Improving outcomes
Professor Enitan Carrol from the Institute of Infection and Global Health at the University of Liverpool, added: “Sepsis is a Department of Health priority, and the software platform will include prompts for the earlier recognition of sepsis, allowing implementation of time-critical interventions to improve outcomes in hospitalised children.”
If successful the aim of the technology is to reduce emergency admissions to critical care.
This will not only be beneficial for patients by targeting treatment earlier and reducing their stay in hospital, but should also prove cost-effective for the NHS.
Programme director for i4i Martin Hunt, said: “Finding faster, more effective ways to identify when young patients are becoming seriously ill is a major challenge – NIHR’s i4i programme funds the development of innovative technology to help solve healthcare problems like this and it’s exciting to see an already effective device for adults being adapted to help improve care for sick children.”