
COVID-19 and our reaction to it have changed our world and, understandably, generated a great deal of anxiety. There are fears that can be addressed with clearer information about who is at risk and why. And, as a starting point, we need to understand how deaths and illness from COVID-19 compare with the normal pattern of disease and deaths in the UK.
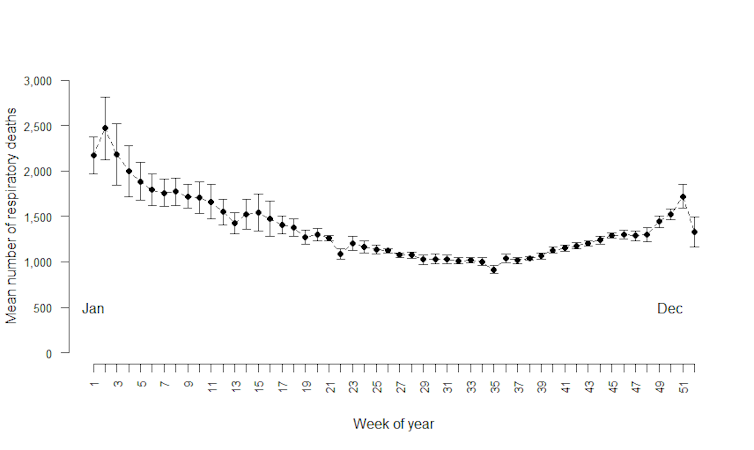
Illness and deaths occur in predictable patterns. For example, deaths from respiratory diseases each year are at their highest during the winter and spring. This historical data can tell us when we are having an abnormally bad year, as in 2015 and 2018 when deaths from respiratory diseases were higher than usual.
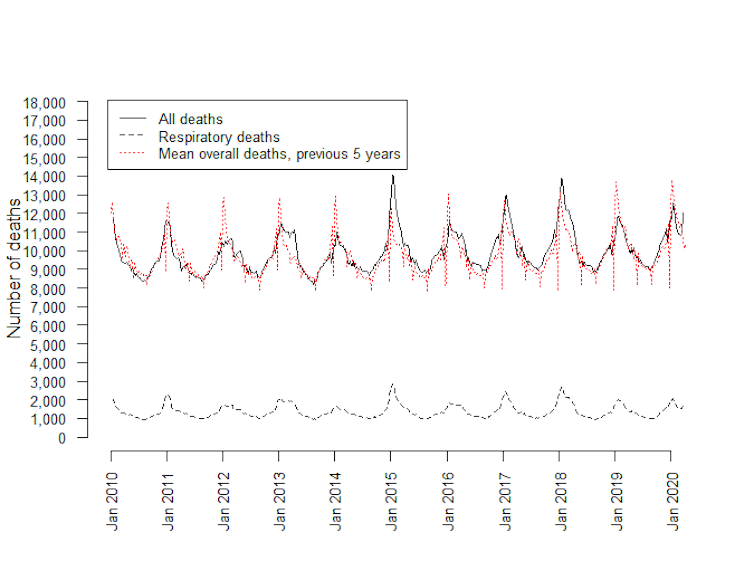
Office for National Statistics licensed under the Open Government Licence
Office for National Statistics licensed under the Open Government Licence
Given the variation in deaths, can we determine whether more people are dying in the UK from COVID-19, compared with the number of deaths from all causes that normally occur?
At the end of March 2020, the pattern of deaths was normal, but in early April the number of respiratory disease deaths (including COVID-19) climbed above the number expected based on historical rates.
At this point in the year the UK usually sees a falls in the number of deaths caused by respiratory diseases – yet both respiratory and non-respiratory deaths have increased in April, in every region of England and Wales. The reduction in all but essential health services, as well as an apparent unwillingness of the public to access healthcare during the lockdown, may affect the number of deaths from all causes of disease. This is something the government might need to consider when deciding about when to relax rules on self-isolation.
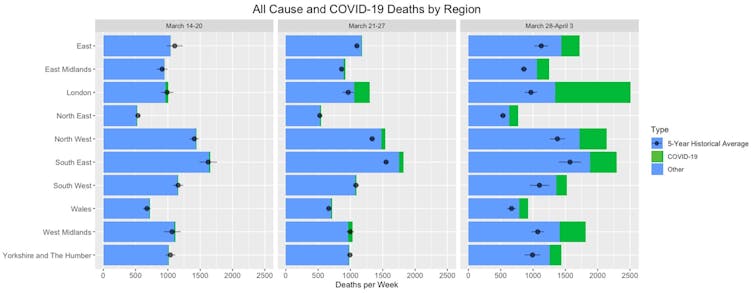
Image developed by Grace Thaxton using data from the Office for National Statistics licensed under the Open Government Licence
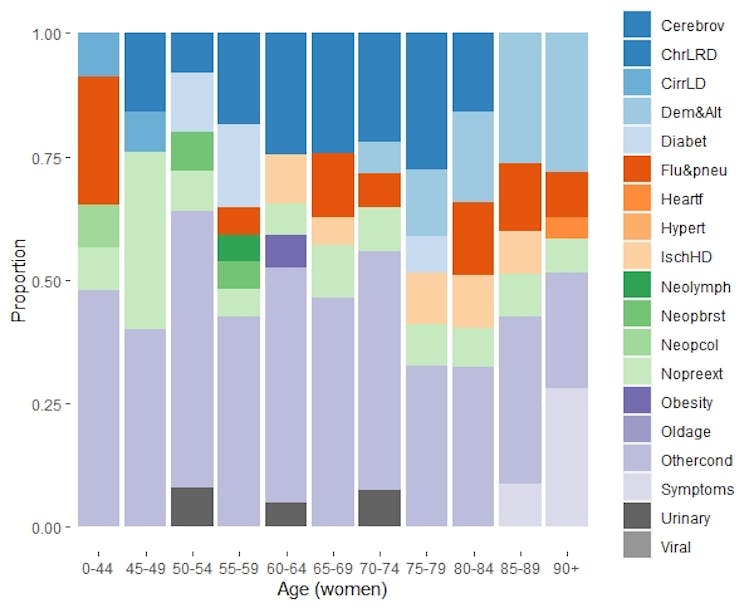
Death rates due to COVID-19 are highest in older people and serious illness and mortality are more common in men. It would be easy to conclude that COVID-19 is a problem mainly in old people and men, yet early information on deaths from this disease suggests that patterns of illness and death mainly mirror what was already happening before the pandemic.
Most deaths (84%) occur in people over 65 years of age and two-thirds (68%) in people over 75 years. When it comes to gender, men die earlier and have a shorter life expectancy at birth (79 years) than women (83 years). The tricky area is understanding the underlying reasons some people die or become more severely ill from COVID-19. To understand what makes certain people more susceptible to this disease, we need to examine the other things that make us ill in the short and long term.
Evidence has emerged that our susceptibility to COVID-19 is related to having an ongoing illness. Everyone gets ill, yet patterns for short and long-term illnesses differ by age. As we age, the odds of having long-term illness increase.
In 2019, a quarter of people aged from 16-44 years old reported a long-term illness versus two-thirds (66%) of people aged from 65-99 years old. The number of chronic illnesses increases with age and many occur earlier in men than women. These patterns together suggest that COVID-19 is a disease of the sick, which is why it appears to be a disease of the old and the male.
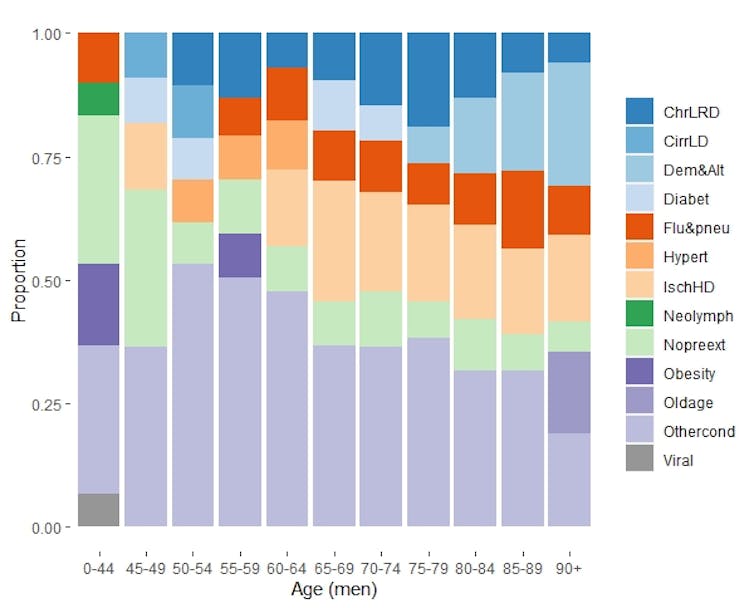
Office for National Statistics licensed under the Open Government Licence
Office for National Statistics licensed under the Open Government Licence
A further complication is that some cases of COVID-19 illness and death in the young and females don’t fit the profile of underlying issues of age and illness. These may be due to high levels of exposure to the virus, which is occurring in hospitals. Careful research on the circumstances behind exposure and on the health of these people will create a better understanding of why they were so badly affected.
Timely data analysis
Policymakers have relied on predictive models in their responses to the early phase of COVID-19. This needs to be supported by timely data analysis of the groups of people most susceptible to this disease, including examining their underlying health conditions.
Information on who and why people get COVID-19 is vital for several reasons. First, we need to understand who is affected in order to assess how the disease, and our reaction to it, affect income generation and the economy as a whole. Second, people need better information on the risks of COVID-19 to manage their own lives and reduce their anxieties.
And finally, the combination of economic evidence and personal wellbeing are needed for future healthcare decisions as the pandemic continues. These aspects are central to planning how best to exit from the COVID-19 lockdown measures, allowing us to return to a cautious normality that will underpin our fragile societies.![]()
Marie McIntyre, Research Associate Epidemiologist, University of Liverpool; Grace Thaxton, Postdoctoral Research Associate, University of Liverpool; Helen Clough, Research Fellow, Statistics, University of Liverpool; John Harris, Lecturer in Public Health and Policy, University of Liverpool, and Jonathan Rushton, Professor of Animal Health and Food Systems Economics, University of Liverpool
This article is republished from The Conversation under a Creative Commons license. Read the original article.