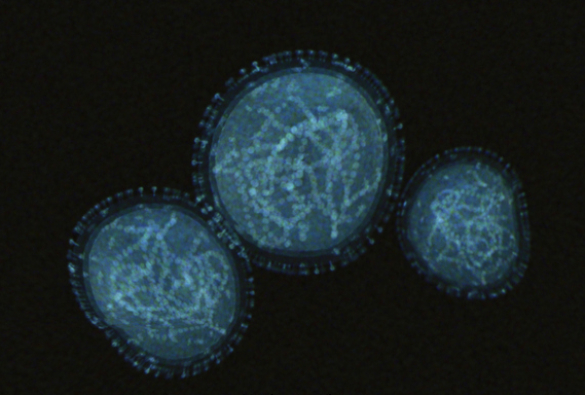
A network of NHS and academic experts from across the country, including the University of Liverpool, has published the results of a timely study looking at the management of previous cases of the human monkeypox virus in the UK by the NHS High Consequence Infectious Diseases Network.
The report, which is published in The Lancet Infectious Diseases, notes that human monkeypox has rarely been seen outside of West and Central Africa. However, in the last five years outbreaks in more densely populated centres have occurred for the first time, with human-to-human transmission well described, raising concerns about its global spread. One such outbreak is the instance we are currently seeing in the UK, where the UK Health Security Agency (UKHSA) defines the virus as a ‘High Consequence Infectious Disease’ (HCID).
Known symptoms of the virus include fever, a characteristic rash, and swelling of the lymph nodes. Complications can include inflammation of the lungs, brain, and eye, which can be sight-threatening, along with secondary bacterial infections. The virus can be dangerous, with estimates of mortality associated with outbreaks in the Congo Basin having ranged from between 1 and 10%, although the West Africa strain of the virus which is responsible for the current UK outbreak has a lower overall mortality.
Nicholas Price of the Directorate of Infection Prevention and Control at Guy’s & St Thomas’ NHS Foundation Trust and Director of the NHS High Consequence Infectious Diseases (airborne) Network is Joint Senior author on the paper. He said: “Until now, monkeypox has been a rare, imported condition in the U.K. and the NHS High Consequence Infectious Diseases Network had treated all seven of the UK’s confirmed cases up until 2021. Outbreaks outside of Africa are unusual but in recent days, significant outbreaks have been reported in several European countries, including the UK, and further afield globally. Clinical trial data is lacking, and we are pleased to share some of our collective experience in managing this previously rare and sporadic condition.”
Using a case-note review, the study looked at the seven cases of human monkeypox, including one young child, which were diagnosed in the UK between 2018 and 2021. The study identified that although limited, transmission within the UK has occurred in household and healthcare settings. All cases had serial monitoring of blood, urine and throat swabs for monkeypox virus by PCR performed at the UKHSA Rare and Imported Pathogens Laboratory. This had never been done before and demonstrated prolonged viral shedding from a variety of body sites, changing our understanding of the biology of this disease.
The patients were managed in specialist HCID centres in Liverpool, London and Newcastle, coordinated via a national HCID network. Their treatment included the first use of antiviral agents in patients with monkeypox, with three receiving brincidofovir and one receiving tecovirimat.
Co-author Calum Semple, Professor of Outbreak Medicine and Child Health at the University of Liverpool, said “This report is useful given the current increase in cases outside of Africa and in the UK in particular. Monkeypox can be serious and affect people of all ages. We hope our experience of managing these people will be helpful and illustrate the particular challenges of caring for affected families with young children.”
First author on the paper, Liverpool School of Tropical Medicine’s Hugh Adler, commented that: “While the study size was small, the data gleaned from the seven cases were rich, providing the team with novel insights and suggesting the direction of travel for future research. We hope this dataset will inform clinicians caring for patients with monkeypox across the UK and Europe, but also in West and Central Africa where there is an unmet need for treatments for this infection. And working collaboratively with the NHS England High Consequence Infectious Diseases (Airborne) Network has been a fruitful experience.”
The authors concluded that while brincidofovir appears to have only limited value as a treatment, further studies of tecovirimat in human monkeypox are warranted, given the observed shorter duration of symptoms and viral shedding in the patient who received this agent compared with the other patients in the series.
The publication of this paper is timely as it highlights that human monkeypox is an emerging global threat, capable of cross-border spread and onward transmission. As such, this virus poses significant challenges even to well-resourced healthcare systems with HCID networks. The study also emphasises the urgent need for prospective studies of antivirals for this disease and that the infection control implications of prolonged viral shedding should be considered in future outbreaks.
The study has been coordinated by the UK’s High Consequence Infection Diseases Network and with support from the International Severe Acute Respiratory and Emerging Infection Consortium and includes authors from: Liverpool School of Tropical Medicine; University of Liverpool; Liverpool University Hospitals NHS Trust; Guy’s and St Thomas’ NHS Foundation Trust, Alder Hey Children’s NHS Foundation Trust; UKHSA; University College London; Newcastle-upon Tyne NHS Foundation Trust; University of Newcastle; Royal Free London NHS Foundation Trust; University of Oxford; Royal Devon and Exeter NHS Foundation Trust; Sheffield teaching Hospitals NHS Foundation Trust; Karolinska Institute, Sweden.
Research reference:
Clinical features and management of human monkeypox: a retrospective observational study in the UK, The Lancet Infectious Diseases, 2022, https://doi.org/10.1016/S1473-3099(22)00228-6