Researchers from the University of Liverpool have been awarded approximately £1.8m to lead a multinational research consortium seeking to define the best and safest treatments for patients who require treatment for tuberculosis (TB) whilst receiving second-line antiretroviral therapy (ART).
The VirTUAL Consortium (Vulnerable patient Tuberculosis AntiretroviraL),which is led by the University’s Institute of Translational Medicine, was funded by the European and Developing Countries Clinical Trials Partnership (EDCTP) as part of EDCTP2 – an international initiative to optimise the safe and effective treatments of poverty related diseases including HIV and TB.
These conditions disproportionally affect the world’s most vulnerable populations including pregnant women, children and adolescents.
Poverty Related Diseases
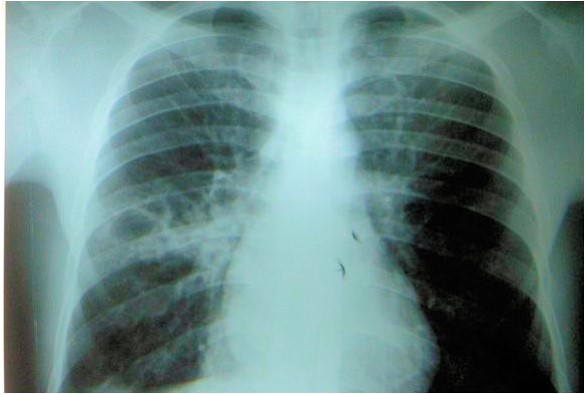
Tuberculosis remains the leading cause of HIV-related deaths. Even whilst on effective antiretroviral treatment, people remain at a four-times increased risk of TB.
Since 2003 there has been great success in the roll out of ART to the populations at greatest need; currently half of the 35 million people living with HIV worldwide are now on treatment. However, despite this success, up to 10% of patients will require second line ART ever year.
There are important drug interactions between the second line ART treatments recommended by the WHO and TB treatments, meaning this population is difficult to treat.
Novel Approach
Global targets to reduce mortality from diseases such as HIV and TB will not be met without a specific focus on populations who are often excluded from clinical trials.
Focussing on the priority research area of TB treatment during second-line ART, the VirTUAL Consortium aims to improve current understanding of drug disposition in complex clinical scenarios and provide a flexible platform for identifying clinical strategies with application to other disease areas; this will have wide-ranging impact in the management of poverty-related diseases in special populations.
Physiologically based pharmacokinetic (PBPK) modelling uses a computational approach to predict the likely doses required clinically, and is increasingly used to design safe and efficient clinical trials.
Dr Marco Siccardi, Senior Lecturer in Pharmacology will be leading this innovative PBPK work and remarks that, “The opportunity of using advanced experimental and computer-based tools to identify optimal therapeutic strategies and in parallel to support the training of scientists in various African countries is an extremely exciting prospect.”
Complex clinical challenges
A dose-escalation study will take place in Uganda, and data collection from pregnant women, children and adolescents requiring TB treatment whilst on second-line ART will be collected from Uganda and South Africa. Population pharmacokinetic modelling will explore the reasons why individuals respond differently to the same dose of drug, and will aim to enable more precise dose recommendations for these populations.
Capacity building, knowledge transfer, studentships and dialogue with stakeholders and communities will take place throughout the five-year programme
Dr Catriona Waitt, Senior Lecturer in Clinical Pharmacology and Lead Investigator on the VirTUAL Consortium, said: “This is an innovative research programme which not only seeks to address an important clinical challenge (TB in patients on second-line ART) but also seeks to equip African researchers with the clinical, scientific and mathematical tools to explore the complex clinical challenges which cause high rates of illness and death in their populations.”
The VirTUAL consortium is led by the University of Liverpool; other members include the Joint Clinical Research Centre (JCRC) and Infectious Diseases Institute (IDI) in Kampala, the University of Cape Town (UCT) and the Desmond Tutu HIV Foundation (DTHF) in Cape Town and the University of Turin.