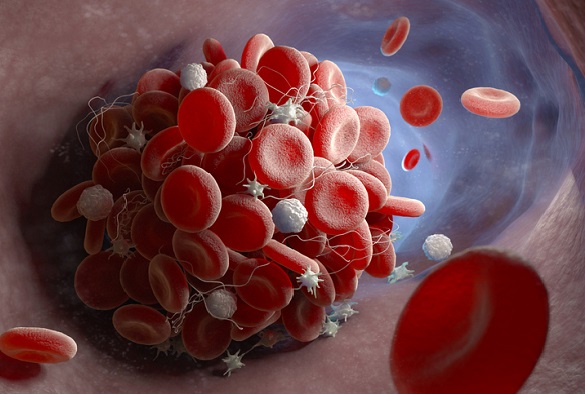
Depiction of a blood clot forming inside a blood vessel
A new international state of the art position document, published in Journal of the American College of Cardiology, highlights the implications of the current coronavirus disease 2019 (COVID-19) pandemic on the prevention and treatment of thrombotic disease patients.
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. The clot may plug a vessel in the lungs (pulmonary embolism), brain (stroke), gastrointestinal tract, kidneys, or leg. Thromboembolism is a significant cause of morbidity and mortality, especially in adults. Treatment may involve anticoagulants (blood thinners), aspirin, or vasodilators (drugs that relax and widen vessels).
COVID-19, a viral respiratory illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), may predispose patients to thrombotic disease to excessive inflammation, endothelial dysfunction, and other complications.
In addition, many patients receiving antithrombotic therapy for thrombotic disease may develop COVID-19, which can have implications for choice, dosing, and laboratory monitoring of antithrombotic therapy.
In an effort to optimize the available technology to care for patients without COVID-19 who have thrombotic disease, a global consortium of international researchers with major expertise in thrombosis, including Professor Gregory Lip, Lead for the Liverpool Centre for Cardiovascular Science (LCCC)/Price-Evans Chair of Cardiovascular Medicine at University of Liverpool, have published this international consensus paper on the current understanding of the pathogenesis, epidemiology, management and outcomes of patients with COVID-19.
The position document also examined those with pre-existing thrombotic disease who develop COVID-19, or those who need prevention or care for their thrombotic disease during the COVID-19 pandemic.
Professor Gregory Lip, said: “Thrombotic disease may be precedent factors or incident complications in patients with COVID-19. Important considerations for the preventive and therapeutic use of antithrombotic agents should be kept in mind to mitigate the thrombotic and haemorrhagic events in these high-risk patients. Funding agencies, professional societies, patients, clinicians, and investigators should work collaboratively to effectively and efficiently address numerous critical areas of knowledge gap.”
This review, which can be found here, is endorsed by the International Society on Thrombosis and Haemostasis (ISTH), the North American Thrombosis Forum, the European Society of Vascular Medicine, and the International Union of Angiology. Supported by the ESC Working Group on the Pulmonary Circulation and Right Ventricular Function.