
Dr Caitlin Robinson is a Lecturer in Urban Analytics at the University of Liverpool and Annika Hjelmskog is a PhD Candidate in Planning at the University of Manchester.
The UK’s COVID-19 vaccine rollout has swiftly offered increased protection to millions of Britons, who are being prioritised largely according to their age.
At a basic level, this makes sense. The UK’s strategy has been to protect its most vulnerable people first, and age is a major risk factor for severe COVID-19. However, this system of prioritisation inadvertently privileges those who are more affluent, and for that reason, it is unfair. Here’s why.
This way of rolling out vaccines overlooks the fact that as social deprivation increases, people on average die younger. For example, in England, the difference in life expectancy between the least deprived and most deprived areas is 9.5 years for men and 7.5 years for women.
This creates a bias towards vaccinating affluent people. As of February 24, in the least deprived 20% of the population, just over 250,000 people over 80 had been vaccinated, along with around 450,000 people aged 70-79. But in the most deprived 20% of the population, only around 130,000 people over 80 and just over 240,000 aged 70-79 had taken a vaccine. This difference is simply down to fewer people who suffer deprivation living to these ages.
If the age risk for COVID-19 was uniform for everyone, this wouldn’t matter so much. But in deprived areas, people are also more likely to have underlying health conditions or simultaneously have multiple diseases – what are known as multi-morbidities – at a younger age. This makes for a stark disparity in healthy life expectancy, too.
Men in the most deprived parts of England can expect 18.9 fewer years of good health compared with those in the least deprived areas, while for women the gap is 19.4 years. In Blackpool, for instance, men and women have a disability-free life expectancy of just 53 and 57 respectively. In Blackpool’s most deprived ward, Bloomfield, healthy life expectancy is just 47 years.
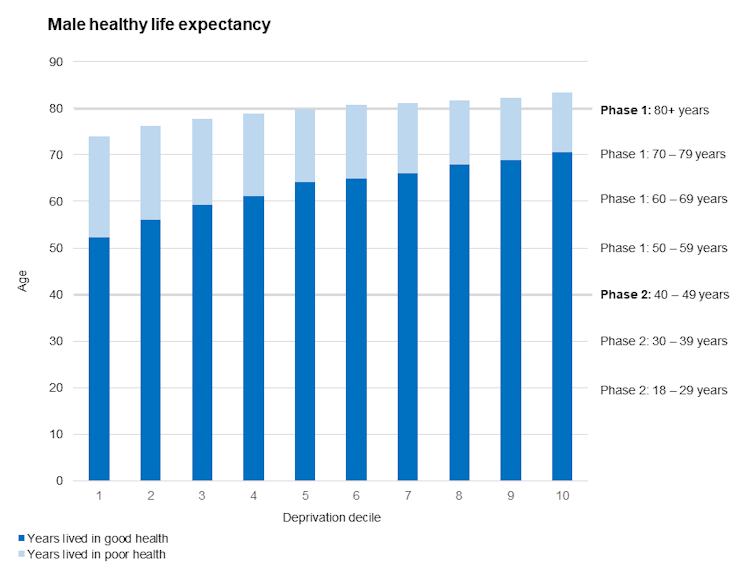
Author provided, based on data from the Office for National Statistics
So while it’s true that the older you are the more susceptible you are to the virus, in more deprived neighbourhoods where overall health is poorer and ill health arrives earlier, vulnerability to COVID-19 will arise earlier too – poor overall health and multi-morbidities drive up the risk of COVID-19. You can see this in the graph above – the vulnerability of poor overall health, shown in light blue, arrives much earlier in life for those in the more deprived groups on the left.
What this means is that people’s vulnerabilities to COVID-19 may be the same, even though their ages – and vaccine eligibility – aren’t. Continuing to vaccinate by age group therefore just adds another layer of health inequality to those that already exist. The rollout should use a relative definition of age that is linked to deprivation to determine who should be vaccinated next. Under this system, a person in the most deprived 10% of the population who is, say, 45 might be considered the same priority as someone in the least deprived 10% who is over 60.
Of course, extremely clinically vulnerable people have already been prioritised, and an additional 1.7 million vulnerable people have recently been added to the priority list. But while this will protect those most at risk, it doesn’t fully cover everyone whose vulnerability is heightened because of their lower healthy life expectancy.
More to equality than prioritisation
The case for focusing on deprivation when rolling out the vaccines isn’t only related to age. People who live in more deprived areas are also less likely to work from home and are more likely to live in overcrowded conditions, which evidence suggests increases potential exposure to the virus. Conversely, more affluent people are more able to protect themselves.
We saw how this played out in the UK’s second wave. As cases surged nationwide, they were consistently higher among deprived populations.
Recent evidence also suggests that when vaccines are offered, there are inequalities in uptake too. Vaccine coverage is lower in deprived areas. As of February 24, in the least deprived 20% of the UK population, 96% of people over 80 had been vaccinated, compared with just 89% in the most deprived 20%. For those aged 70-79, the difference in coverage was 95% among the least deprived 20% compared with 88% among the most deprived.
This suggests that any attempt to get the vaccine programme to respond to health inequalities needs to focus on more than just how people are prioritised. Lower uptake in certain groups poses a risk to both individual and population health and is likely to act cumulatively with existing deprivation measures to exacerbate disadvantage.
Lower uptake in more deprived groups may be down to a need to boost vaccine confidence among them. Equally, it could be because people who suffer greater deprivation have reduced access to mainstream health services. Extra effort is needed to see if these or other factors are at play and to lessen their effects.
The COVID-19 vaccine has great potential to mitigate some health inequalities if it is delivered with more intense effort in places that are more vulnerable overall. But without taking deprivation into account, we risk doing the opposite: widening the gap even further between the least deprived and the most deprived.
The vaccine rollout should now specifically target those inequalities in deprivation and health that COVID-19 has so dramatically highlighted. As well as helping those who are most deprived, ultimately, this will benefit everyone. We have already seen that the UK’s most deprived areas have had the most difficulty in suppressing infection rates, and has widely been noted, in a pandemic no one is safe until everyone is safe.![]()
This article is republished from The Conversation under a Creative Commons license. Read the original article.