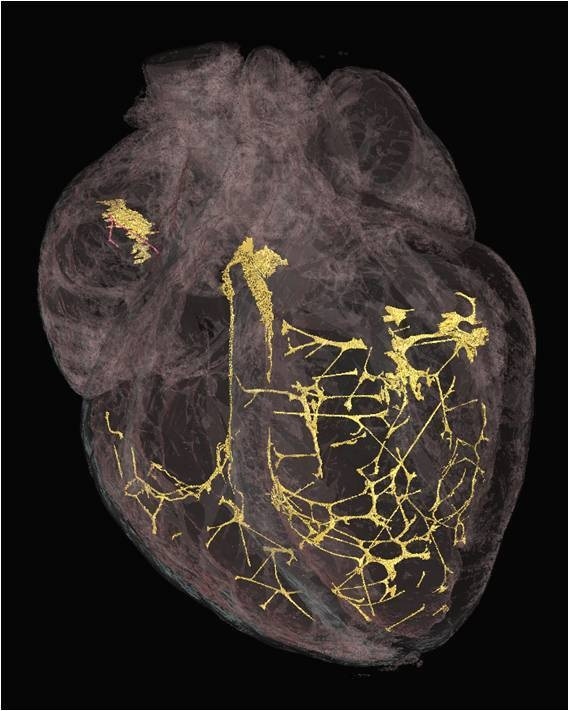
Scientists at the University have developed a new X-ray technique to identify tissue fibres in the heart that ensure the muscle beats in a regular rhythm.
The new 3D images could further understanding of how the body’s heartbeat can be disturbed, which may help medics develop ways to reduce the risk of fibrillation – a condition in which heart muscle contracts chaotically and fails to pump blood rhythmically around the body.
The heart needs to pump blood in a regular rhythm to maintain a steady circulation of blood to all parts of the body. It does this through the coordinated action of the muscle tissue, that pumps the blood, and the conducting tissue, which is necessary to distribute an electrical wave to trigger every heartbeat. Until now scientists have been unable to produce high resolution 3D images of the conducting tissue to fully identify the network that controls heart rhythm.
The team at Liverpool used a micro CT scanner to image hearts that had been treated with iodine to highlight the different parts of the tissue. They found that the solution was absorbed less significantly by the conducting parts of the heart compared to the muscular parts of the organ, allowing scientists to clearly identify the areas that produce electrical activity on the resulting 3D image.
Dr Jonathan Jarvis, from the University’s Institute of Ageing and Chronic Disease, said: “These new anatomically-detailed images could improve the accuracy of future computer models of the heart and help us understand how normal and abnormal heart rhythms are generated. 3D imaging will give us a more thorough knowledge of the cardiac conduction system, and the way it changes in heart disease.
“Computer models based on these high-fidelity images will help us to understand why the heart rhythm is vulnerable to changes in heart size, blood supply, or scarring after a heart attack. One of the major concerns for surgeons in repairing malformed hearts, for example, is to avoid damage to the tissue that distributes electrical waves. If they had access to 3D images of the conducting tissues in malformed hearts, however, it could be possible to understand where the conducting tissue is likely to be before they operate.”
The research, in collaboration with Alder Hey Children’s Hospital and the University of Manchester, is published in PLoS ONE.
That’s fascinating. Is the Micro CT scanner here in Liverpool or is it with your collaborators?
all the scanning so far has been done on the excellent equipment at the Henry Moseley X-Ray Imaging Facility at the University of Manchester.
Jonathan
I applaud to you and your team on this breakthrough. I am keen to see this applied in clinical practice especially during Cox-Maze Radio-frequency Ablation Surgery to control re-entry rhythms and atrial fibrillation. We perform these cardiac surgical proc. and can’t have a visual aid to predict its efficiency and efficacy. Yet, I am hopeful that such technology might be able to give us a clue of what we have ablated on the conducting tissue.
Thank you Mohamad.
There is a long way to go before we could imagine clinical use of such techniques. However, I do believe that such high resolution anatomical data will enhance the predictive ability of virtual models. That should mean that our understanding of the common re-entrant circuits, and perhaps the sources of AF, will be improved.
What is the total X-ray exposure required to produce these images. Thanks.
We cannot calculate the radiation dose exactly from our data, but as an estimate its probably in the range of several hundred mGy. For this study it was not in our interest to make the procedure clinically viable but it is something we would like to work towards.
If you are interested in the kV, mA and exposure times they are all available in the publication- http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0035299
Is that also able to reveal where premature ventricular contraptions originate from in the heart,especially during ablation?
The anatomical data alone does not allow us to predict where premature ventricular contractions might arise. However, we are working with colleagues in Manchester University (Boyett/Zhang) to combine this new data with their models of action potential generation. This will improve the existing virtual models, and these do have the potential to predict where arrhythmias are most likely to be generated.
Is this using Hologic Tomosynthesis?
It is using micro computed tomography, which is similar to the technique known as tomosynthesis in that it uses images taken at many angles through the tissue to make up a 3 dimensional image.
However, hologic tomosynthesis uses the changes in X-ray attenuation in, for example, breast cancer tissue to make the image. That does not work for the conducting system of the heart. The basis of the visualisation we have used is to add a contrast agent (in this case iodine) to create differential X-ray attenuation.