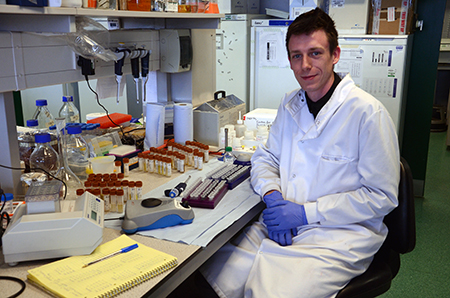
 PhD student, Nicholas Ellaby is sequencing bacteria from the samples to try and find clues which point to the prime factors in the gut which cause necrotising enterocolitis (NEC)
PhD student, Nicholas Ellaby is sequencing bacteria from the samples to try and find clues which point to the prime factors in the gut which cause necrotising enterocolitis (NEC)
Parents of new-born children are used to dealing with their child’s dirty nappies, but not to the extent of the dedicated scientists at the University of Liverpool who are in receipt of over 13,000 faecal samples from premature babies.
The researchers are using the samples, which are stored in more than 25 fridges at the University’s Institute of Integrative Biology, to search for clues to the cause of a serious bowel condition that affects thousands of premature infants in the first few weeks after they are born.
Using a variety of techniques, including genetic sequencing and gas chromatography mass spectrometry, the researchers are looking for patterns in the bacterial makeup of the children’s stools to find the causes of necrotising enterocolitis, more commonly abbreviated to NEC.
This is a serious illness in which tissues in the intestine become inflamed and start to die. This can lead to a perforation developing, allowing the contents of the intestine to leak into the abdomen. Treatment is usually in the form of antibiotics, but doctors are sometimes forced to resort to intravenous feeding to rest the intestine, or an operation to repair the gut, which requires the baby to be put under general anaesthetic.
Receiving samples from around the country
At Liverpool, the team receives samples from specialist baby units in the Midlands, Yorkshire and Merseyside. Each sample comes accompanied by a wealth of information including the age, the type of milk ingested and the gender of the baby as well as the date the sample was produced and the medication they are on. There are also notes on twins, triplets and even one set of quadruplets.
All of these are entered into a database which then uses software developed at the University to find the best matches. For every sample sent for a baby with NEC, there are two which are NEC free and used as controls. The database groups the best matches so that, as far as possible, the only difference is the fact that one baby has NEC and the others don’t.
There are two strands to the research which is then carried out. In the first, Nicholas Ellaby, a PhD student in the Institute of Integrative Biology, is sequencing the bacteria from the samples to try and find clues which point to the prime factors in the gut which cause NEC.
“The bacterial makeup of the gut is extremely complex,” Nicholas says. “But what we’re predicting is that there will be a pattern in babies with NEC and it’s only by working with a large number of samples that we can gather enough data to identify this.”
Getting the DNA
Getting the results is a painstaking process as each sample needs to have the DNA separated from the rest of the faecal matter. Even this DNA is a mixture of bacterial and intestinal DNA, so this also needs to be separated.
Using the facilities at the University’s Centre for Genomic Research, Nicholas first chemically softens the stools before washing them in alcohol and attaching the DNA to fibres by spinning the solution in a high speed centrifuge. He analyses a specific section of ribosomal proteins unique to bacteria, enabling him to see which species are present in NEC and NEC-free samples.
Nicholas adds: “Finding patterns by sequencing individual bacteria produces much more data than we need, but by looking at groups of bacteria which operate together, we can find patterns. There is likely to be a group, or several groups, acting together to cause NEC in babies.
“The findings from this study could have a major impact on developing drugs and treatments for a relatively common, but very serious illness.”
The smell of illness
Meanwhile in the University’s Institute of Translational Medicine another side of this project is also well under way. Anecdotal reports from nurses have suggested that there is a distinct smell that comes from NEC faeces, so scientists in this area are attempting to prove this using the same set of samples used by Nicholas in the genomics department.
Using gas chromatography mass spectrometry, scientists are seeking out the volatile organic compounds (VOCs) which are particular to NEC faeces to aid in diagnosis on the hospital ward. These are produced by the bacteria. At the moment the only clues doctors have to identify NEC is spotting some of the most common symptoms – which include tenderness in the stomach, vomiting or blood in the stool. Since these symptoms show when the disease is already quite advanced, there is a real need for earlier identification.
By creating an artificial ‘nose’ that can accurately detect the VOCs associated with NEC, doctors will be able to act much more quickly.
Arnaud Mayor says: “We’ve got a lot of experience in this department of creating detectors which can identify smells. The technology is already proven for detecting cancer and if we can find the right smells for NEC, we can adapt the technology to improve detection here too.”
Working together, the two departments are pooling their expertise and comparing results, so that the outcomes of the research can help treat NEC in babies at the early stages of detection and by making a cure much less invasive.
At the cutting edge of science, this project is also helping to understand much more of what is living in the gut and how it gets there from the day we are born.
Find more news on genomics at Liverpool here, and find out more about study options in this field on the University’s Study Pages.