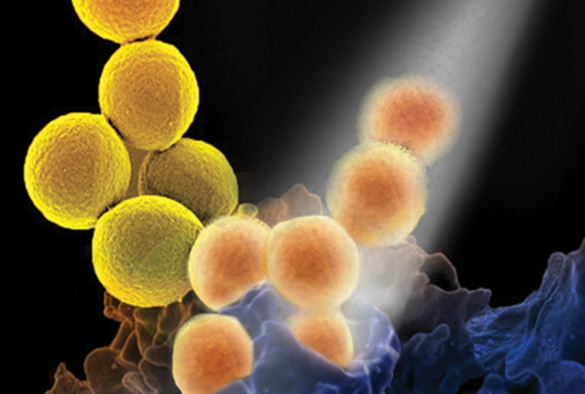
Image courtesy of NUI Galway
Microbiologists have identified how MRSA may be more effectively treated by modern-day antibiotics, if old-fashioned penicillin is also used. The team from the University of Liverpool and the National University of Ireland Galway have shown that, although penicillin does not kill the bacteria, it does weaken their virulence, making it easier for our immune system and other antibiotics to eradicate the infection. The research findings, funded by the Health Research Board and the Medical Research Council, are published in the Journal of Infectious Diseases.
MRSA infection is caused by a type of Staphylococcal bacteria that has become resistant to many of the antibiotics used to treat ordinary infections. This results in significant morbidity and mortality with up to 20% of patients infected with MRSA dying from systemic infections.
Escalating crisis
Study co-lead Professor Aras Kadioglu, from the University’s Institute of Infection and Global Health, commented: “Although aggressive hospital infection control initiatives appear to be having a positive impact on hospital-acquired MRSA rates in some developed countries, the global burden still remains unacceptably high. Infections caused by community associated MRSA strains and strains that are currently methicillin sensitive are increasing at a worrying speed. Given the escalating antimicrobial resistance crisis, it is imperative to identify new therapeutic strategies and to re-evaluate how current antimicrobial drugs are used, as such our data are timely and highly important.”
Professor James O’Gara of the National University of Ireland Galway commented: “Our findings explain the anti-virulence mechanism of penicillin-type antibiotics and support the re-introduction of these drugs as an adjunct therapeutic for MRSA infections. MRSA can be extremely virulent, which is part of the challenge in treating it. Our laboratory research shows that when exposed to penicillin, the bacteria switches off its toxin genes and instead concentrates on thickening its cell wall to resist the antibiotic. Our immune systems can then take advantage of this compromised state to destroy the bacteria.”
Potential to change guidelines
This new treatment strategy for MRSA infections has the potential to change the current clinical guidelines for treatment of patients with MRSA infections in both hospital and community settings. A recent randomised controlled trial in Australia involving 60 patients led by Menzies School of Health Research showed that the beta-lactam antibiotic flucloxacillin in combination with vancomycin significantly reduced the duration of MRSA sepsis from 3 days to 1.9 days.
“The clinical findings in Australia are very important and now we have the key laboratory data that help explain why the combination of two antibiotics is better than one. The beauty of this approach is that penicillin type antibiotics are not only widely available and safe, but can potentially and more easily be included in clinical practice without the need for long and expensive clinical trials needed for new drugs,” added Professor O’Gara.
Graham Love, Chief Executive at the Health Research Board commented: “This research demonstrates the potential payback having a vibrant health research programme. It clearly has the potential to change clinical practice and improve outcomes for patients.”
Antimicrobial resistance (AMR) is one of the greatest current threats to human health. The recent report commissioned by the UK Government, concluding that AMR infections will cause more deaths than cancer by 2050 if not addressed urgently.
The paper ‘Redeploying β-Lactam Antibiotics as a Novel Antivirulence Strategy for the Treatment of Methicillin-Resistant Staphylococcus aureus Infections’ is published in the Journal of Infectious Diseases and is available to view here.