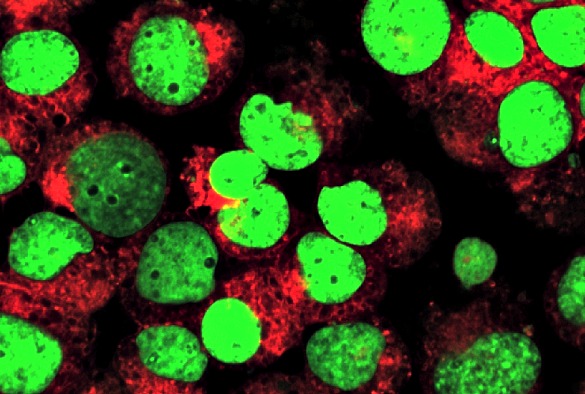
Leukemic cells labeled with fluorescent molecules
New University research, presented at an international conference, confirms that a novel approach to the treatment of chronic myeloid leukaemia (CML) can safely increase treatment success and reduce negative side effects.
Drug treatment for CML is with tablets called tyrosine kinase inhibitors (TKIs). These have drastically improved the prognosis for CML patients, essentially turning what was a deadly cancer into a chronic disease with normal life expectancy for most patients, which can be managed with a daily pill.
Traditional advice to patients with CML is that their drug medication must be lifelong. But common side effects include chronic headaches, stomach problems and fatigue, and women are typically advised not to conceive children while taking the drugs due to the high risk of birth defects.
De-escalation and cessation
This has led some patients and their doctors to question whether it would be feasible to discontinue their use after a patient achieves consistently negative leukaemia test results.
Now, the results of a new study called DESTINY suggest that many CML patients may have improve their chances of successfully stopping treatment by reducing the amount of medication before stopping therapy all together.
The new research, led by Professor Richard Clark from the University’s Institute of Translational Medicine, examined whether patients with excellent responses to their treatment could first reduce the amount of medication (de-escalation) and then completely stop therapy (complete cessation) without reactivation of the disease but with reduction of adverse side effects. Importantly, the study deliberately included patients with low but still detectable leukaemia, who have not been previously studied in trials in other countries.
Remissions
174 patients (98 male and 76 female) were recruited after giving informed consent from 20 UK centres. At entry, patients were receiving one of three TKI leukaemia drugs (148 imatinib, 16 nilotinib and 10 dasatinib) for an average of approximately seven years.
During the first 12 months of half dose de-escalation, 98% of patients with virtually undetectable leukaemia and 81% of those with low detectable levels remained fine but with improvement in their side effects.
Now, Professor Clark and his team report that in the subsequent 12 months of complete treatment cessation in 117 stable patients, only 26 further recurrences and four withdrawals occurred, giving a recurrence free survival (RFS) rate of 76% for the overall 24 months for this patient group. And 39% of the patients with low level detectable leukaemia remained fine overall, again with improvement in side effects.
All the patients whose leukaemia recurred were rapidly returned to deep remissions when they resumed their TKI treatment, confirming that if carefully supervised, attempting to stop treatment carries little if any long term risk to the leukaemia control.
Improvement
Professor Richard Clark, said: “TKI de-escalation is safe for most CML patients with stable and excellent responses to TKI therapy after some years of treatment, and is associated with improvement in symptoms.
“Overall our findings are better than any other studies world-wide, and imply that our unique gradual withdrawal of treatment might be important. We don’t yet understand why our results are so good, but this is a happy problem to have!”
Dr Alasdair Rankin, Director of Research at the blood cancer research charity Bloodwise, said: “Since their introduction, TKI drugs have transformed the lives of people with CML, enabling many to live a relatively normal life simply by taking tablets every day. But treatment is life-long, and some people will experience serious side effects that severely impact their quality of life.
“The results of this study so far are really encouraging, and suggest that under careful monitoring, many people who are doing well on their TKI may ultimately be able to reduce or even stop taking their medication. But this study is not complete and reducing or stopping treatment will not be right for everyone, so it’s really important that patients with CML talk to their doctor before considering any change to their medication.”
The study, entitled ‘Initial reduction of therapy before complete withdrawal improves the chance of successful treatment discontinuation in Chronic Myeloid Leukemia (CML): Year 2 results in the British Destiny Study’, can be found here.
The findings were presented by Professor Clark at the European Haematology Association conference in Madrid on Saturday, 24 June.